What is Osteoarthritis?
Osteoarthritis (OA) is the most common degenerative joint condition affecting between 2% and 3% of the population and 80% of those over the age of 50.
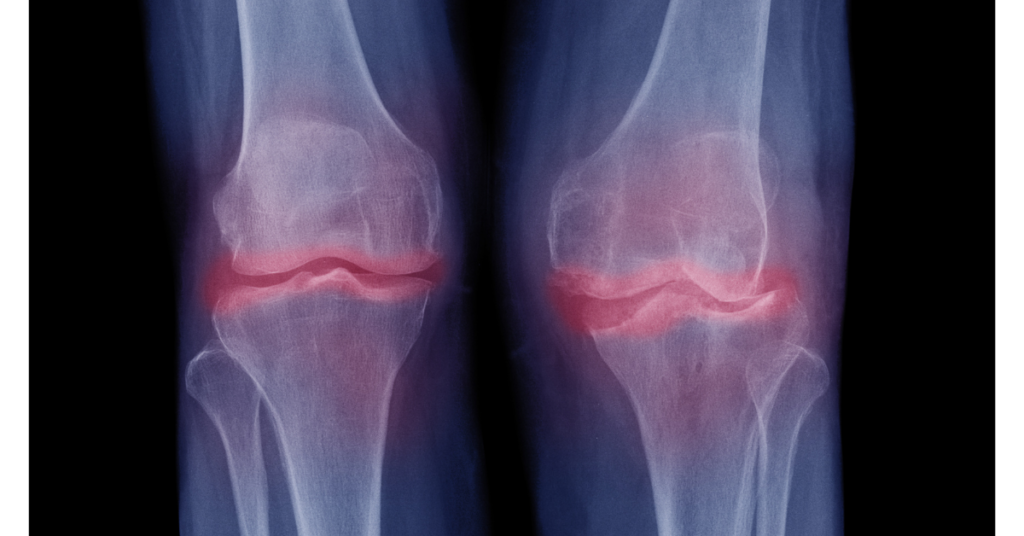
It is characterised by a degeneration of the articular cartilage, synovial membrane, and eventually the bone next to the cartilage.
OA can affect all the joints of the body, but is most commonly found in the hands, knees, hips, and spine.
A breakdown of the cartilage matrix leads to cracks and ulcers and a thinning of the cartilage with a loss of shock absorption.
The underlying bone starts to thicken as a response to the increasing stress resulting in the formation of bony spurs.
In the advanced stages of osteoarthritis, an inflammatory reaction in the synovial membrane can be seen.
Predisposing factors include:
Having parents with a history of OA.
Being overweight.
Previous injuries or overuse.
Under-use of joints.
Symptoms include:
Pain or / and stiffness in or near a joint, improves with activity.
Bony swelling in a joint.
Conventional Treatment Strategies
Topical Pain Relief (applied to the skin)
Includes creams, sprays, and rubs that can be applied directly to the skin. There are many different preparations available from the chemist; these tend to contain salicylates, skin irritants, or capsaicin. If using capsaicin preparations, use for at least 2 to 3 weeks as it takes this long to work properly.
Oral Analgesics
Paracetamol: Often the first drug to be prescribed, especially for the elderly or patients with a history of peptic ulceration / bleeding problems. It is more effective when taken regularly.
Nonsteroidal anti-inflammatory drugs (NSAIDS): Used to treat the pain of arthritis as well as helping to reduce inflammation. Most common NSAIDS drugs include ibuprofen, aspirin, voltarol, and naproxen. If you develop any signs of stomach irritation, inform your doctor immediately.
Corticosteroids: A doctor can give these synthetic substances by direct injection into the affected joint. This helps to reduce pain and inflammation for a number of months.
Surgery
Most people with arthritis will not need to have surgery. Surgery is reserved for severe, disabling cases of arthritis when other treatments have failed. Surgery may be done to prevent the joint from becoming deformed, to correct a deformity, to remove bone material from around the joint to allow for greater movement, or to replace a damaged joint with an artificial one.
Symptoms include:
Crackling noises on moving a joint
Poor range of movement and joint instability
Diagnosis is based on:
Medical history and examination by a doctor.
Blood tests to rule out inflammatory causes.
X-rays of the affected joint.
(See also our articles on Arthritis and Rheumatoid Arthritis)
Complementary Treatment Strategies
The following information does not constitute a prescription or recommendations – this is included for your information only.
Self Help – Pain Diary
Keeping actively involved in the management of your arthritis will increase the effectiveness of any treatment regime.
Recording details such as pain levels, amount of swelling, types of activity attempted, what you can and can’t do, and noting unusual changes in symptoms will be a great help in monitoring your progress.
Biochemical Strategies
Diet and Nutrition
You need sulphur-containing foods to repair and rebuild your bone, cartilage, and connective tissue.
Foods high in sulphur include asparagus, eggs, garlic, and onions.
Eat less saturated fat and more alkaline-forming foods like millet, organic fruits and vegetables.
Other good foods are green leafy vegetables, fresh vegetables, non-acidic fresh fruit (avoid oranges, plums, and rhubarb), whole grains, oatmeal, and brown rice.
Food Avoidance
Certain foods may trigger a flare-up of arthritis in certain individuals, and should be avoided.
They are dairy products, gluten (as found in wheat, oats, barley, and rye), corn, sugar, and members of the nightshade family (potatoes, tomatoes, eggplant, peppers, and tobacco).
Reduce your intake of acid-forming foods such as tea, coffee, alcohol, red meat, biscuits and cakes.
You may want to check for other food allergies and food intolerance as well (especially if you have rheumatoid arthritis).
Natural Supplements
Glucosamine Sulphate: Clinically proven to provide pain relief. Take 500 mg (with food) 3 times daily for 30 days. Glucosamine sulphate may take 4 to 10 weeks to produce noticeable results. Ideally take in combination with:
Chondroitin Sulphate: Take 500 mg (with food) 3 times daily. Chondroitin sulphates inhibit the enzymes that destroy joint cartilage and collagen.
Essential Fatty Acids: These work by inhibiting the prostaglandins that cause pain and inflammation. The most potent fatty acid is GLA (gamma linoleic acid) available in evening primrose oil, borage oil, and black currant seed oil.
Bromelain: An enzyme from the pineapple plant, is especially effective in reducing the inflammation from arthritis.
Herbal Therapy
Ginger can give you significant pain and inflammation relief. Take 100 mg daily in supplement form, or include fresh ginger in your diet.
Turmeric (referred to as curcumin) has the strongest anti-inflammatory activity of all herbs. Take 200 mg of curcumin once or twice daily.
Boswelia is anti-inflammatory in action, and is very effective in treating arthritis and other inflammatory conditions. Take 400 mg-800 mg daily in divided doses, with meals.
Structural Strategies
Exercise
Always consult with your doctor prior to commencing any exercise program.
Keep moving: Exercise is an excellent way to prevent and treat arthritis. The keys are to not over stress your joints, and to work within your limits of tolerance.
Exercise’s many other benefits to mind and body include:
Reducing stress.
Enhancing sleep.
Improving your physical capabilities.
Promoting relaxation.
Increasing your resistance to disease.
Improving sexual function, satisfaction.
Preventing joint deformities.
Helps to achieve optimal weight.
Always discuss with your doctor about trying and combining a combination of stretching exercises, mild strengthening exercises (such as lifting weights) and low-impact aerobic exercises (such as swimming, walking, or bicycling).
Energy Strategies
Magnet Therapy
Magnet therapy represents one of the cheapest and most widely available forms of energy therapies available. Used by healers for more than 3000 years and thousands of arthritis sufferers worldwide is can for some, but not all people provide a good level of pain relief.
How it works is controversial, one theory, however, is that applying static magnets activates the body’s natural healing mechanisms by helping cells to regain their natural electromagnetic field.
Microcurrent Therapy
A new generation of TENS machine has emerged called ACE. This innovative pain relief system delivers a phased programme of microcurrents designed to mimic the body’s natural electrical currents and in doing so stimulate tissue repair and regeneration. The claimed benefits are:
Instant pain relief.
Increased joint and muscle mobility.
Injury heals faster and stronger.
Reduction in swelling.
Good night’s sleep.
Acupuncture
Has been clinically proven to help with the symptoms and pain control of people with arthritis.
Psycho-social Strategies
Meditation
Focusing on a particular object produces a state of ‘relaxed awareness’ that reduces stress and perception of pain. (See also Visualisation).
Relaxation
Spend more time on activities that relax you. For example listening to music can have a temporarily beneficial effect on blood pressure levels.