What is Diverticular Disease?
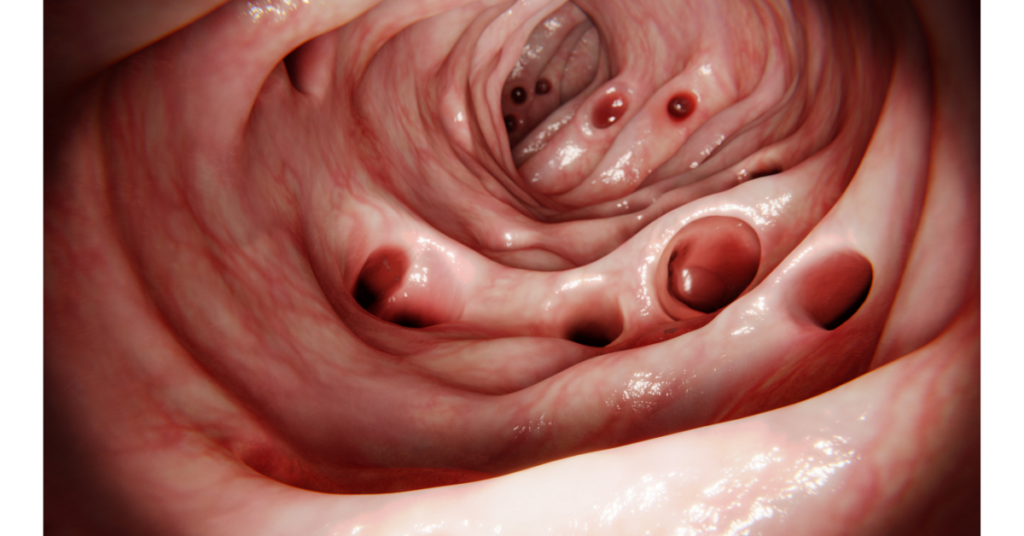
Diverticular disease is a condition affecting the large intestine, caused by inflamed or infected diverticula – small bulges or pouches that develop in the colon wall.
The condition of having diverticula (known as diverticulosis) is very common amongst the older generation of industrialised nations, affecting about 50% of people over the age of 60 in the US alone.
When the pouches become infected or inflamed (due to waste matter becoming trapped in them), the condition is called diverticulitis (this occurs in about 10-25% of people with diverticular disease).
Signs and symptoms
Diverticulosis
Many people with diverticulosis don’t have any symptoms. Others may have mild cramps, bloating, and constipation.
Diverticulitis
Symptoms include abdominal pain (especially tenderness around the left side of the lower abdomen), cramping, bloating, fever, nausea, vomiting, chills, and constipation or diarrhoea. Blood in the stools may also occur, although this is relatively uncommon. Diverticulitis can also lead to complications such as abscesses, perforation, peritonitis (an infection that spreads into the abdominal cavity), fistulas (abnormal passages that connect one loop of intestine to another, or even to other organs), and intestinal obstructions.
Causes
A low-fibre diet is seen as a major cause of diverticular disease, because it often leads to constipation, which in turn can cause pouches to form in the weak spots of the colon wall due to the excess pressure required to force small, hard, and dry stools through the bowel. Stress, smoking, obesity, coronary heart disease, gallbladder disease, and a family predisposition towards the disorder are also believed to increase one’s chances of developing diverticulosis / diverticulitis later in life.
Diagnosis
A barium enema: A procedure in which the colon is filled with liquid barium and X-rays are taken.
Sigmoidoscopy: A thin, flexible lighted tube is inserted into the rectum to enable the doctor to look at the lower colon.
Colonoscopy: This is similar to a sigmoidoscopy, except that it allows a view of the entire colon and rectum.
Conventional Medical Treatment
Drug therapy: Antibiotics are commonly used to treat diverticulitis during the early stages of an attack. Pain relievers or drugs such as propantheline (Pro-Banthine) may also be utilised to control muscle spasms in the colon.
Surgery: For more severe or frequent attacks. Surgery involves the cutting open of the abdomen and removing the affected part of the colon. The remaining parts of the colon are then rejoined.
Complementary Medical Treatment
Dietary therapy
A high fibre diet is recommended. This is an approach that most conventional doctors also advocate. The drinking of plenty of good quality water is also advised. Major irritants to the gut such as dairy products, red meat, sugar, fried food, spices, and processed foods are best avoided. Nuts, seeds, and grains (except for well-cooked brown rice products) should also be cut out since they are hard to digest and tend to therefore get caught in the crevices of the colon wall, leading to bloating and gas.
Supplements
Psyllium husk is a great bulk and stool-softening fibre. However, do not overuse laxatives as they can irritate the gut wall. Probiotics can help repopulate the gut with friendly bacteria to help fight of infection / inflammation.
Herbs
Alfalfa contains vitamin K and various minerals that are often deficient in people with intestinal disorders. It is also high in chlorophyll, which helps to detoxify the system.
Aloe vera can help to reduce inflammation.